July 30, 2018
Bioengineered human 'pseudoislets' aim to improve treatments for type 1 diabetes

University of Calgary researchers have developed a way to reorganize clusters of human pancreas cells — islets — in order to give them a better chance of survival when transplanted into people with type 1 diabetes.
Normally, cells within the islets continuously monitor the amount of glucose (sugar) in your blood, and if there is too little or too much, the cells release hormones that increase or decrease it accordingly. When the levels get too high, islet beta cells release insulin, a hormone that tells cells throughout the body to absorb glucose. Type 1 diabetes is caused by a loss of these cells. Patients have to test their blood sugar throughout the day and inject insulin to try to compensate, but this can cause discomfort, and their constantly changing blood sugar levels can lead to long-term health problems.
“One way to treat type 1 diabetes is to transplant islets isolated from the pancreas of an organ donor,” says Dr. Mark Ungrin, PhD, associate professor of comparative biology and experimental medicine in the Faculty of Veterinary Medicine. “The current process was developed by our collaborators in Edmonton, and is known internationally as the ‘Edmonton Protocol’." Ungrin is pictured above, right, with his PhD student Yang Yu.
'Edmonton Protocol' process helps patients but isn't a complete cure
With the Edmonton Protocol, doctors inject the donated islets into the liver. Over the years the process has helped hundreds of patients with diabetes become less dependent on insulin. But it isn’t a complete cure. Many islet cells don’t survive the transplantation because the cells in the middle don’t get enough nutrients and oxygen, particularly in larger islets.
Ungrin, who studies how cells work together to assemble into tissues and organs, has previously invented a microscale tissue engineering technology called AggreWell. This technology — used by researchers around the world — assembles cells into clusters with controlled size and composition, allowing cells to help each other survive and function, without having to compete for limited oxygen and nutrients.
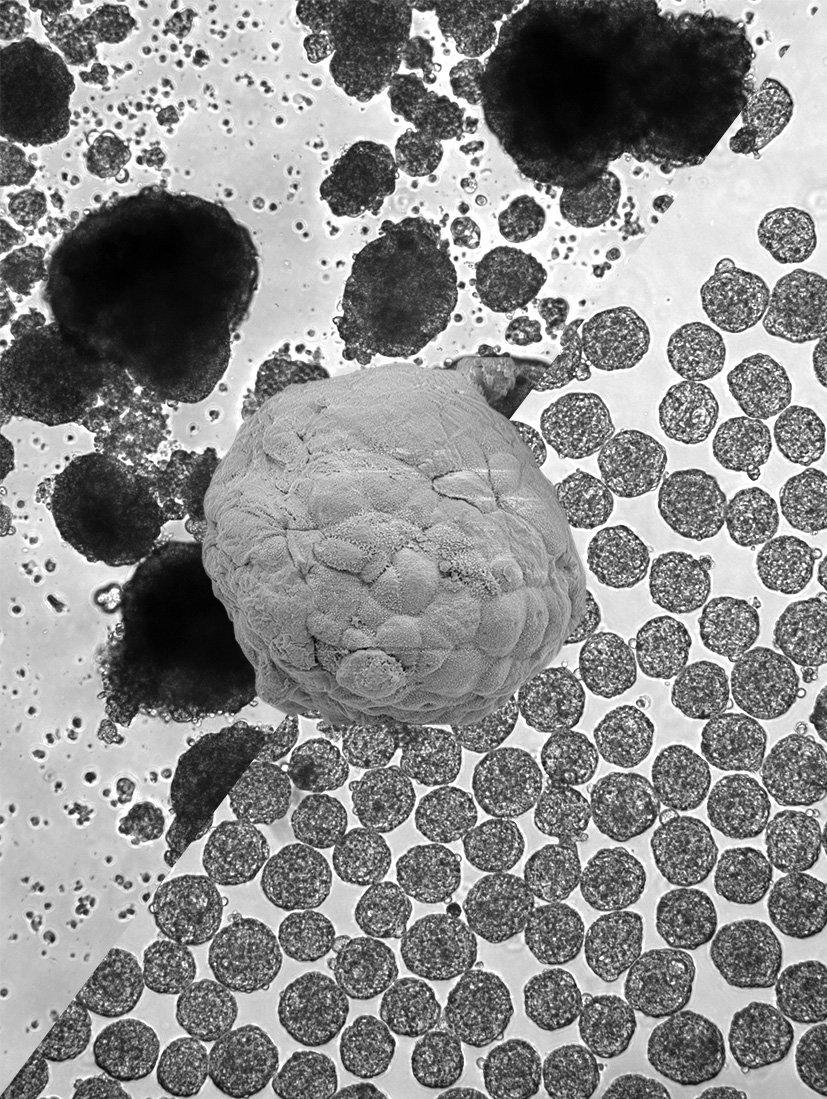
Light micrographs of human islets (top-left) and engineered human pseudoislets (bottom-right).
Yang Yu and Mark Ungrin
- Above: Light micrographs of human islets (top-left) and engineered human pseudoislets (bottom-right), with an electron micrograph of a single human pseudoislet centred.
PhD student drove 'up and down the QEII to Edmonton' a lot to get the research done
Working with the researchers who developed the Edmonton Protocol at the University of Alberta, Ungrin and his PhD student Yang Yu used AggreWell to engineer "pseudoislets" that are better suited for transplantation. “Once we had shown the effectiveness of our approach in the lab, we needed to verify that it would work in a transplant setting,” says soon-to-be Dr. Yu, who recently successfully defended his PhD thesis, largely based on this research. “I spent a lot of time driving up and down the QE II to Edmonton and back to do experiments in the Shapiro and Korbutt labs.”
The research was published in Diabetologia, the journal of the European Association for the Study of Diabetes.
“Our engineered pseudoislets perform very well in the lab, and in mice,” says Ungrin. “Over the next few years we plan to establish the scale-up and quality control necessary to bring the approach to the clinic. In this paper we focused on donated human islet material since that’s what’s most commonly used in patients at present. However, the approach has been designed so when stem cell-derived pancreatic cells become available and receive approval, we can substitute them to alleviate the shortage of organ donors.”
The paper’s co-authors include Edmonton Protocol pioneers, Drs. James Shapiro and Greg Korbutt, both professors in the Department of Surgery at the University of Alberta.
How you can participate in a research study at the University of Calgary

“Our engineered pseudoislets perform very well in the lab, and in mice,” Mark Ungrin says.
Riley Brandt, University of Calgary.
Funding for this study was provided by the Canadian Institutes of Health Research, the Alberta Diabetes Institute/Alberta Diabetes Foundation, the University of Calgary University Research Granting Council, and the Diabetes Research Institute Foundation of Canada.
Ungrin is a supervisor in the Biomedical Engineering Graduate Program, a member of the Alberta Children’s Hospital Research Institute, and is affiliated with the Alberta Diabetes Institute, McCaig Institute for Bone and Joint Health, Centre for Bioengineering Research and Education, and the Arnie Charbonneau Cancer Institute. Yu is a graduate student in the Biomedical Engineering Graduate Program, and was supported by an Alberta Diabetes Institute Graduate Studentship.
